Americans face distinct challenges in accessing affordable health care. A good chunk of the blame lies with public policy, which has historically not only failed to invest in health care’s supply side but has often actively restrained it. This commentary focuses on the nation’s inadequate supply of physicians. Attempts at limiting physician numbers have harmed patient well-being while failing to achieve the ostensible goal of reducing overall health spending. By restricting the supply of physicians, health care spending has instead been redirected towards more intensive and specialized medical services at the expense of primary care and broader patient access. In order to redress these mistakes, the United States should pursue policies aimed at substantially boosting the number of physicians.
Access to health care is worse than in other countries
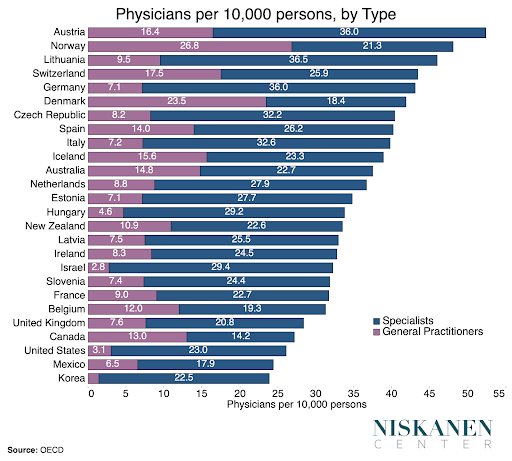
Relative to comparable countries, Americans generally report greater difficulty accessing care across a variety of survey metrics. The number of physicians per person is a fairly reliable proxy for the number of service access points within a health system, and on this measure, the United States is on the bottom rung. The U.S. physician deficit holds up even accounting for other autonomous medical roles such as nurse practitioners, both because such practitioners are less numerous than physicians and because equivalent positions exist to varying degrees in other countries. Largely as a result, over 80 million Americans live in medically underserved areas where access to basic primary care is exceedingly scarce.
The rise of U.S. medical supply restraints
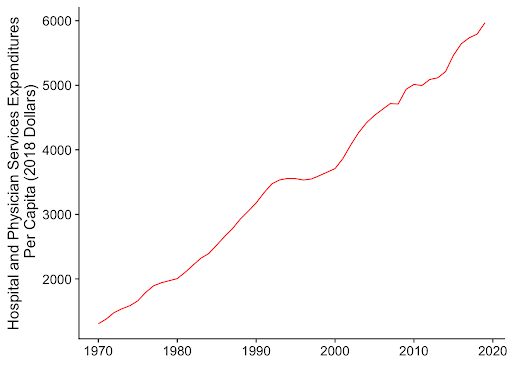
Public policy is the primary driver behind the United States’ restricted supply of physicians, driven by misguided reforms aimed at controlling costs. In the postwar years, spending on health care ballooned as new and more complex procedures reached an ever-wider swath of the public. The United States was near the top among developed countries in growing the number of physicians to deliver these services.
With quality medicine becoming more widely available than ever before, policymakers began to worry about growing costs and the demand on public dollars. The rise in the number of physicians quickly came under scrutiny as a contributing factor. In 1959, Milton Roemer found that the number of hospital beds available to a population correlated positively with the number of days spent in the hospital across that population. The hypothesis that “ultimate control over money spent for hospitalization, therefore, is the volume of beds provided in the community” — often summed up as “a hospital bed built is a bed filled” — came to be known as Roemer’s rule. Around the same time, academic economists became increasingly interested in the asymmetry in medical knowledge between physicians and the patients they treat. By the early 1970s, economists formalized these insights into theories of “physician-induced demand,” which hypothesized that greater physician competition would push doctors to use their medical authority to overtreat patients. Evidence for this theory, as with Roemer’s law, was based upon naive associations between statistical aggregates, in this case between physician density and measures of health care consumption.
By the 1980s, reports by the U.S. government were warning of an imminent “physician surplus,” resulting in the withdrawal of federal support for medical students and residencies. Nongovernmental actors in the physician pipeline heard the message loud and clear, raising the stringency of residency requirements and instituting a moratorium on medical enrollment at MD-granting schools in order to curb the number of U.S. physicians.
With the benefit of hindsight, it’s clear that the evidentiary link between widespread physician-induced demand and health care costs was weak. Although increased physician density generally translates into increases in the total quantity of services performed by physicians, the early studies failed to differentiate between increased availability of valuable medical services and unnecessary treatment and services. In reality, the greater utilization in places with more doctors represented greater availability, both in terms of expanded access to primary care and an ever-growing array of new and more advanced medical services. The impact of physician-induced demand on levels of treatment now appears to be small. And where overtreatment does happen, an oversupply of doctors is unlikely to be the culprit. Even early on into the “surplus” concerns, researchers were puzzled by the growing divergence between the U.S. and Europe’s physician supply. Indeed, the only high-quality field experiment looking precisely at supplier inducement in the healthcare industry found that provider density didn’t explain patterns of overtreatment.
Why physician-supply restraints backfired
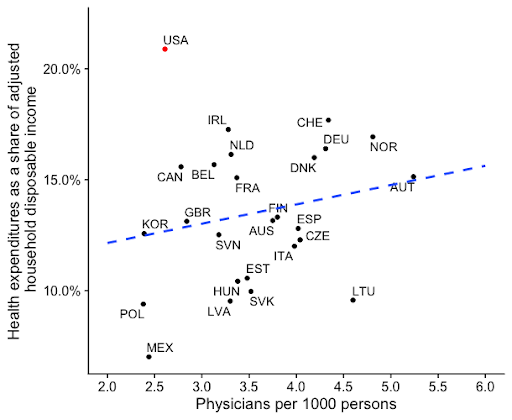
Restraining particular features of the supply side, such as the number of physicians, has little bearing on overall health care spending. That is, holding demand constant, restraining the number of physicians mostly appears to shift the costs to different and less valuable parts of the health system.
The evolution in thinking on “certificate of need” (CON) laws, which limit the construction of new medical facilities, is informative here. In 1974, the federal government mandated that states enact CON laws in order to control the growth of health spending. Yet this mandate was repealed in 1987 following the realization that costs were simply migrating to other forms of spending, such as outpatient clinics. The accumulated body of evidence since the mandate’s repeal suggests that if CON laws have any impact on costs, it’s actually to raise them. Tellingly, modern supporters of CON laws defend them on the basis of controlling hospital quality, rather than the original cost-control rationale.
The connection between physician density and health care costs is exceedingly tenuous. That isn’t because physicians don’t cost money, but because when physicians are scarce, the money simply gets spent elsewhere in the health system. All indications are that squeezing physician supply is much like squeezing a balloon — the costs largely migrate rather than disappearing altogether.
Physician-supply restraints backfired by making health care services less accessible for ordinary Americans. Face time with a physician is generally critical to obtaining health care services, yet their availability is in increasingly short supply. The Affordable Care Act’s expansion of healthcare coverage to millions of Americans thus didn’t increase the overall amount of health services provided. With intrinsic barriers to the supply of providers, services just went to different people. As a result, pushing more money through a healthcare system with highly limited capacity simply results in increased intensity of per-patient care. That is, when doctors are in short supply, medical providers are encouraged to squeeze more dollars from each patient in the form of more intensive procedures, excessive diagnostic testing, and by offering more non-medical amenities.
The intensive nature of American medicine is evident in our exceptionally high utilization of diagnostic imaging tests, such as MRIs, PET, and CT scans. Overuse of these technologies is worrying on multiple levels. It’s been estimated that the number of patients receiving potentially dangerous exposure to radiation through CT scans is higher in the United States than in any other developed country. In fact, up to 2 percent of cancers in the U.S. may be attributable to this excessive radiation exposure. And even when diagnostic tests in themselves aren’t harmful to patients, they can encourage overdiagnosis and overtreatment of essentially benign conditions, introducing additional risks. Analyses thus find that U.S. health care spending is overwhelmingly driven by technological factors which increase the cost and intensity of care without necessarily improving outcomes.
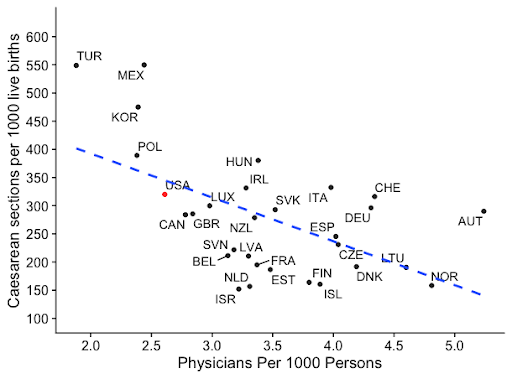
Looking at the medical procedures themselves, cesareans are the most common operating room procedure in the country, accounting for 8.8 percent of all such procedures and one-third of all births. The procedure can be lifesaving when medically necessary, but overuse of the procedure introduces significant risks to both the mother and child. The procedure itself costs, on average, roughly 40 percent more than a vaginal birth, while the risk of rehospitalization within the 30 days following a cesarean is 230 percent higher. Because of the risks, medical experts generally put the ideal rate of cesarean utilization between 10 and 15 percent—substantially below the rate in the United States. Countries with fewer physicians per person are more likely to over-utilize optional procedures, however, due to the number of competing demands upon a physician’s scarce time. This generates pressure to squeeze out higher levels of revenue per patient. Cesareans are a particularly illustrative example, as physicians value the speed of the procedure despite its risks given the time that it saves. As such, the frequency of c-sections tends to spike at the start of the workday, and decline in prevalence on weekends when the demand on physicians lessens.
The gearing of the U.S. physician workforce towards more intensive care is also evident in America’s exceptional degree of specialization. Despite having fewer physicians per person, the U.S. has a higher proportion of specialists than any country measured by the OECD apart from South Korea. Yet it is not only the breadth of specialization that sets the U.S. physician workforce apart, but the depth of specialization as well. The number of distinct specialties and subspecialties in the U.S. is substantially greater than in other countries surveyed by the UK’s General Medical Council. The growth in the number of U.S. physicians pursuing post-residency fellowship training, which doesn’t even exist in many countries, is thus a product of our limited physician supply. Physicians cannot be in multiple places at the same time, so providers are encouraged to compete on the basis of intensity in order to maximize revenues for their hospital or private practice.
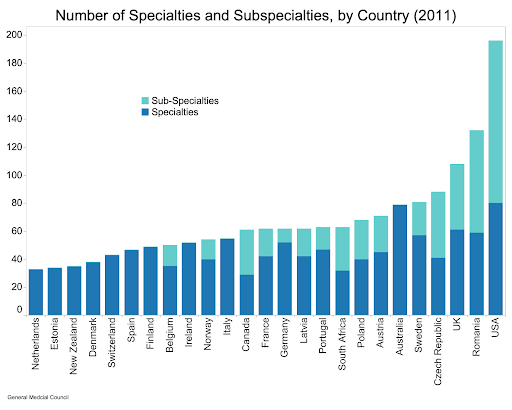
The value obtained from such extreme physician specialization is dubious. Although most studies imply that specialists perform better at discrete medical procedures, the density of specialists actually worsens performance on metrics of quality collected by Medicare, in addition to creating far higher costs. This suggests specialists often engage in unnecessarily intensive and expensive care, crowding out nonspecialist providers who offer more basic and beneficial medical services and harming overall population health in the process.
Keeping physicians so specialized that their services barely overlap also limits the potential for competition to check prices. Physicians operating in areas with lower levels of competition as measured by the Herfindahl-Hirschman Index have higher incomes, even after controlling for a variety of physician characteristics, including age and specialty. Indeed, competition among providers may be especially important to cost control in the United States given our reliance on decentralized, uncoordinated insurers. The short-lived “managed care revolution” of the 1990s, during which insurers heavily micromanaged physician services, was the only event in U.S. history to have noticeably reduced the rate of healthcare spending growth at the level of national aggregates.
The collapse of managed care-driven price competition led to the revival of retail competition strategies, resulting in non-care-related patient amenities playing a larger role in hospital demand. Retail competition in health care is inherently problematic from the standpoint of medical quality. Analyses suggest that hospitals that invest in amenities such as “private rooms, healing gardens, atriums, waterfalls, and WiFi” are able to capture market share, driving out those that invest in medical quality and harming patient mortality in the process.
We would expect these dynamics to result in basic health services remaining scarce for typical Americans in spite of ever-more spending, which is exactly what the country has experienced over the last 40 years.
Increasing the number of physicians would improve American health care
Restricting physician supply appears not only to have failed in terms of controlling costs, but likely also delivered a health care system that’s comparatively worse at ensuring the health of U.S. citizens. This is because more basic medical services are generally recognized to have a far greater impact on population health than specialized ones. And those high-impact, basic medical services are what become scarce as a result of supply restrictions.
The density of physicians has been routinely found to be associated with better health outcomes. The density of primary care physicians is associated with lower mortality. Similarly, the density of specialists has often been found to be associated with reductions in mortality from specific diseases. For example, death rates from melanoma decrease with an increase in the density of dermatologists. Patients seem to like being in places with a greater availability of physicians, too. Density has been found to be positively associated with a variety of patient-reported outcomes, such as physical and mental health status.
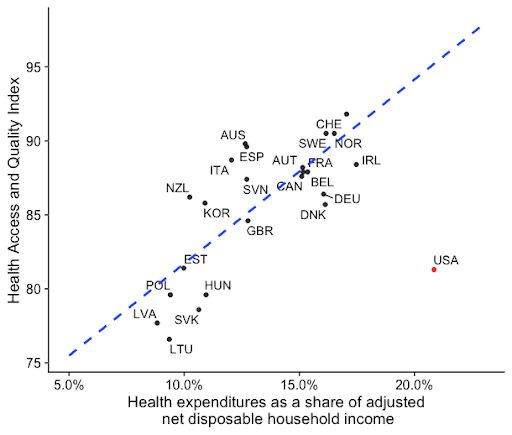
There is a consistently positive relationship between health expenditures and health outcomes across most other countries. The U.S. departs from this trend. Although we spend substantially more than any other country, our outcomes lag substantially. One way to view the United States’ relative underperformance is by looking at the Health Care Access and Quality Index in the chart below, which measures avoidable deaths.
Drawing an analogy with housing, another supply-constrained market, limits on physician numbers are much like minimum lot sizes in the housing market. If a developer is unable to maximize the use of their land, they will tend to build more expensive, luxury housing that commands a higher price per square foot. Physician supply constraints have had a similar effect, shifting doctors away from primary care and into lucrative specialties. Neither policy places meaningful restraints on aggregate costs. Instead, they may actually encourage excess consumption by those who have access while reducing basic access for others — access that is actually far more valuable in terms of promoting better public health outcomes.
The answer is more doctors
Increasing the number of U.S. physicians would allow our current health spending to be used more productively. Encouraging medical providers to squeeze as many dollars as possible out of each encounter does not improve patient outcomes, and may actually be harmful. Making the most basic forms of medical care more available has the highest potential benefit for American patients, and increasing physician numbers provides a clear recipe for doing just this.
The first step to increasing physician supply is to increase the generosity of federal residency funding, which has been capped since 1997. Yet it’s just as important for the federal residency financing system to be reformed in order to get our money’s worth, ensuring that the residency system trains the right mix of specialists and in the places where they are most needed. Smart investments to construct or expand teaching hospitals and medical schools in areas that are currently underserved would also make sense.
The geographic tilt of physicians towards wealthier metropolitan areas is often pointed at in order to argue that the current physician supply of physicians is, in fact, sufficient. Some amount of urban bias exists in all rich countries, but increasing overall physician numbers will clearly benefit currently underserved communities. Data going back to the 1960s shows that while the geographic distribution of physicians is far from uniform, it has diffused to smaller and smaller communities as the national level of physician density has increased. This is consistent with the activation of market forces, with physicians filtering out of more populated areas as competition increases. Furthermore, more physicians enables greater competition among medical providers, granting insurers greater leverage to manage sources of waste and unnecessary care. Given that the U.S. population is relatively more dispersed, the number of physicians necessary to ensure health care access that is comparable to other rich countries is likely higher.
Bottlenecks in the physician training pipeline are largely the result of previous policy choices and are restraining the supply of U.S. physicians. Yet the case for restraining the physician supply is incredibly weak. A “surplus” of physicians will exist when prospective medical students forgo the profession in favor of more attractive opportunities. Given our current shortcomings in access, the United States thus has little to lose and much to gain from increasing the supply of physicians across the board.


 (-1 rating, 1 votes)
(-1 rating, 1 votes)